Hip Replacement Surgery at Berkshire Independent Hospital
What is a hip replacement?
A hip replacement is an operation that replaces a worn or damaged hip joint with a new prosthetic (artificial) hip joint.
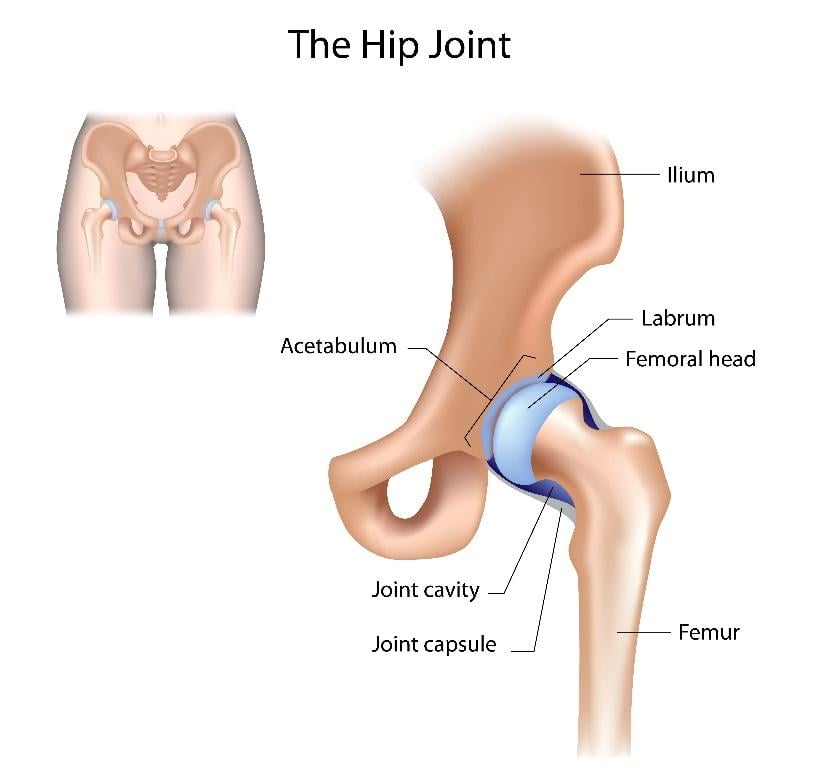
The hip joint is a ball and socket joint. The ball of the joint (called the femoral head) sits at the top of the long thigh bone in your upper leg (the femur). It fits into a socket (called the acetabulum) formed by the bones in your pelvis.
Hip replacement surgery involves removing both the ball and the socket and replacing them with a prosthetic ball and socket made from metal, ceramic or durable plastic. The hip operation is performed under general, epidural or spinal anaesthetic.
Discover more about the procedure with our guide 12 Things You Need to Know About Hip Replacement Surgery.
Why go private for a hip replacement?
One of the major advantages of going private for your hip replacement is that your appointments and treatment times can be arranged to suit you, without any unnecessary waiting. This can be especially important if you need to avoid particular dates for surgery, or if you’re in a lot of pain.
At Ramsay Health Care, you’ll be treated by a highly regarded and experienced orthopaedic surgeon of your choice, with a special interest in hips. They’ll discuss your needs and will recommend the best prosthesis for your situation.
Types of hip replacements
During a hip replacement operation, your surgeon will remove the worn and/or damaged bone from your hip joint and replace it with a prosthetic hip joint.
The new hip joint can be made from a variety of materials, including:
- Metal-on-plastic: A metal ball with a hard plastic socket. This is the most widely used combination of materials
- Ceramic-on-plastic: A ceramic ball with a hard plastic socket
- Ceramic-on-ceramic: A ceramic ball and socket. Ceramic is hard-wearing and often used in younger and more active patients
The parts of your artificial hip joint can be held in place by:
- Medical cement: Your prosthesis is secured to healthy bone using acrylic cement
- An uncemented placement: The surfaces of your prosthesis can be treated and roughened to encourage bone to grow onto it and keep it in place. This method is long-lasting and becoming more common, especially in younger, more active patients
- Hybrid placement: Where only one piece of the joint is cemented into place
Broadly, there are three types of hip replacement surgery:
Total hip replacement
The most common type of hip replacement surgery. With a total hip replacement, the surgeon will replace your entire hip socket, removing both the ball (femoral head) at the top of your thigh bone (femur) and the socket in your pelvis (acetabulum).
Partial hip replacement
These are rarer than total hip replacements. With a partial hip replacement, the surgeon only removes part of your hip joint. This could be just the ball (femoral head) at the top of your thigh bone (femur), just the socket in your pelvis (acetabulum), or even just part of the socket.
Hip revision
A hip revision operation is performed to remove a previously implanted artificial hip joint that has failed or is causing problems. All or part of the old prosthetic is removed and then replaced with a new prosthetic hip joint. Hip revisions can be more complex than total hip replacements and can take longer to recover from.
How do you know if you need a hip replacement?
You may need a hip replacement if your hip joint becomes worn, damaged or diseased over time. If this causes your cartilage (the smooth coating at the end of your bones) to wear away, the underlying bones can become exposed and rub together as you move, causing stiffness, pain, and reduced mobility.
Hip replacement symptoms
Signs you may need a hip replacement include:
- Persistent hip pain that pain medication doesn’t help with
- Pain that worsens with walking, even with the help of a stick or walking frame
- Pain that disturbs your sleep
- Difficulty walking and moving, especially walking up and down stairs
- Difficulty standing up from a seat
At first, you might visit your GP if you’re experiencing persistent hip pain and stiffness. Your GP may carry out a physical examination and request X-rays and blood tests to diagnose the problem.
Your GP may recommend non-surgical treatments to begin with, such as non-steroid anti-inflammatory drugs (NSAIDs) or refer you to a hip surgeon to discuss your options.
What conditions may lead to needing a hip replacement?
Any condition that causes wear or damage to the bones and/or cartilage in your hip joint can lead to you needing hip replacement surgery, whether that’s a disease, an injury, or arthritis.
The most common conditions that lead people to need a hip replacement are:
Osteoarthritis
This is a common condition in people who are ageing. With osteoarthritis, the cartilage that coats the end of your bones wears down over time, causing pain, stiffness, swelling, and reduced movement as your hip bones rub against each other. Osteoarthritis often results from general wear and tear over time, but it can also result from past injuries.
Rheumatoid arthritis
A type of arthritis caused by your immune system mistakenly attacking the healthy tissues lining the inside of your hip joint, resulting in the loss of cartilage and bone over time.
A hip fracture
A break in the top of the thigh bone (femur), usually caused by a fall or accident. This is more common in older patients with weaker bones, especially those with osteoporosis.
How long does a hip replacement last?
How long a hip replacement lasts will depend on a range of factors, including your age, weight, level of activity, any other conditions you might have, like osteoporosis, and the type of hip replacement you’re given.
However, every hip replacement done in the UK is registered on a database called the National Joint Registry (NJR). From the NJR we have a rough idea of how long hip replacements can last - usually at least 15 years in most patients, but as long as 20 to 30 years in others.
Benefits of a hip replacement
Hip replacements are procedures with high rates of success and most patients experience significant improvements in their quality of life, including:
- A significant decrease in hip pain and stiffness
- Better sleep
- Increased range of motion in the joint
- Improved mobility and independence
- The ability to perform daily tasks again, including climbing stairs
- The ability to return to previous hobbies and sports, like walking, cycling, and swimming
- Improved quality of life
How long does a hip replacement procedure take?
Depending on the details of the operation, hip replacement surgery usually takes one to two hours.
Hip surgery is performed under a general or spinal anaesthetic, or with an epidural. Your anaesthetist will discuss your options and recommend the most appropriate for you.
What happens before hip replacement surgery?
Once your hip surgery is booked, you’ll be asked to prepare for your operation. This may include:
- Doing your best to lose excess weight
- Being as active and fit before your surgery as you can (low-impact exercise is best, like walking and swimming)
- Eating a balanced diet
- Reducing your alcohol intake (don’t drink any alcohol for at least 48 hours before your operation)
- Stopping smoking
- Assessing your medication – your consultant will advise if you should continue taking your regular medications before surgery
Read more about a hospital stay with Ramsay, including what to do before you come to us.
What happens during hip replacement surgery?
Once you’re in the operating theatre and under anaesthetic, your surgeon will make an incision (a cut) along the side of your hip. They will remove the damaged ball and socket joint and shape the remaining bone to fit the prosthetic joint.
The prosthetic parts will be attached to your bones using either medical cement, an uncemented placement, or a mix of both. Then, the surgeon will close the incision and bind it using stitches.
Hip replacement recovery week by week
Recovery from a hip replacement varies from person to person, but here’s a general timeline:
What happens the first few days after hip replacement surgery?
You will be encouraged to start walking using an aid, such as crutches or a walking frame. Once ready, you’ll be discharged home.
Two to six weeks after your hip replacement
You should be able to walk more easily and do light daily activities. You may switch to a walking stick or even walk without support. You may be able to engage in gentle exercise and you should be able to go back to work if you have a desk-based job,
Six to 12 weeks after your hip replacement
You should regain more strength and mobility and will likely start walking again without any walking aids. As you approach 12 weeks, you may be able to drive and engage in a range of exercises.
Three to six months after your hip replacement
Significant healing will occur during these months. Most patients feel considerably better and can engage with their lives much more than they could before their hip surgery.
One year after your hip replacement
You should have fully recovered, with good muscle strength and joint function.
Read more about what to expect after a hip replacement and getting fit after a hip replacement.
Potential risks and complications of hip replacement surgery
Hip replacements are common surgeries and usually very successful, but as with any operation, they do carry the risk of complications, such as:
- Pain
- Swelling
- Stiffness
- Scarring
- Nerve damage
- Muscle weakness
- Damage to blood vessels
- Infection of the surgical wound
- Issues with the prosthesis, including it loosening, wearing out, or dislocating
- Bone fractures (broken bones) around the prosthesis
- Bone forming in the muscles around your hip
- Leg length discrepancies
- Excessive bleeding
- Blood clots in your legs (deep vein thrombosis) or lungs (pulmonary embolism)
- Heart attacks
- Strokes
If you think you might be developing any symptoms of complications after your hip replacement surgery, you should seek medical attention right away.
Alternative hip treatment options
Often, people experiencing hip stiffness and pain won’t need a hip replacement and their condition can be treated using alternative methods, such as:
- Lifestyle changes: Including losing excess weight, eating a healthier diet, and exercising more
- Using walking aids: Like a walking stick
- Physiotherapy: To help stretch and strengthen your hip joint and the surrounding muscles
- Corticosteroid injections: To reduce inflammation, stiffness, and pain
- Other medications: Like NSAIDs and painkillers of various strengths
- Other surgical options: Like hip arthroscopy, a kind of keyhole surgery where surgeons can examine your joint and repair or remove damaged tissues
How much does a hip replacement cost?
Hip replacement surgery costs will vary depending on the type of hip surgery you have total or partial), the hospital, and how you choose to pay for your hip replacement.
If you’re self-funding your hip surgery, you can pay with a single, one-time payment at a pre-agreed price with our all-inclusive TotalCare package, delivering direct access to all the treatment you need. We offer a range of other ways to self-fund your hip operation, including 0% payment plans.
Alternatively, if you want to pay for your hip replacement surgery with your private medical insurance, Ramsay Health Care can work directly with your insurance provider to arrange the payment. We recommend you check directly with your insurer that your hip surgery will be covered by your insurance policy before booking your operation with us.
Hip Replacement Surgery with Ramsay Health Care
At Ramsay Health Care we have a wealth of experience in delivering high-quality hip replacements carried out by experienced consultants throughout our more than 40 private hospitals across the UK.
We aim to provide rapid and convenient appointments for the diagnosis and treatment of your hip problem and to offer you the best care throughout your hip replacement journey, so that you can get back to living your life.
Contact us to find out more about hip replacement surgery with Ramsay Health Care.

