Haemorrhoidectomy at Ashtead Hospital
Haemorrhoids, also called piles, are swollen veins in your bottom that can be internal or external. They’re extremely common, affecting up to a third of the UK population, and can vary in severity.
Severe haemorrhoids can be painful and distressing to live with. A haemorrhoidectomy – a surgical procedure to remove haemorrhoids – can be an effective treatment to remove them, especially when other haemorrhoid treatments haven’t worked. While recovery can take several weeks, the majority of patients achieve excellent, long-term relief from their haemorrhoids.
Here, we explain more about what causes haemorrhoids, the symptoms of haemorrhoids, and what a haemorrhoidectomy involves, including what happens during the procedure and what you can expect during recovery.
What is a haemorrhoid?
Haemorrhoids are swollen veins in and around your rectum (the final part of your intestines) and anus (your opening) that become enlarged. Think of them as like varicose veins, but in your bottom rather than your legs.
While many haemorrhoids are mild and resolve on their own, they can be uncomfortable and cause itching, pain, and bleeding, especially after bowel movements. Generally, the worse the haemorrhoids are, the worse the symptoms.
Types of haemorrhoids
Haemorrhoids can be either internal or external:
External haemorrhoids - These develop under the skin around the anus. They can be itchy and potentially quite painful, especially if a blood clot forms within them (a thrombosed haemorrhoid), which can result in a firm, bluish lump forming in the vein.
Internal haemorrhoids - These develop inside the rectum. Internal haemorrhoids are usually painless but can cause bleeding, and in some cases, they can prolapse, bulging out of the anus.
The grading system for internal haemorrhoids
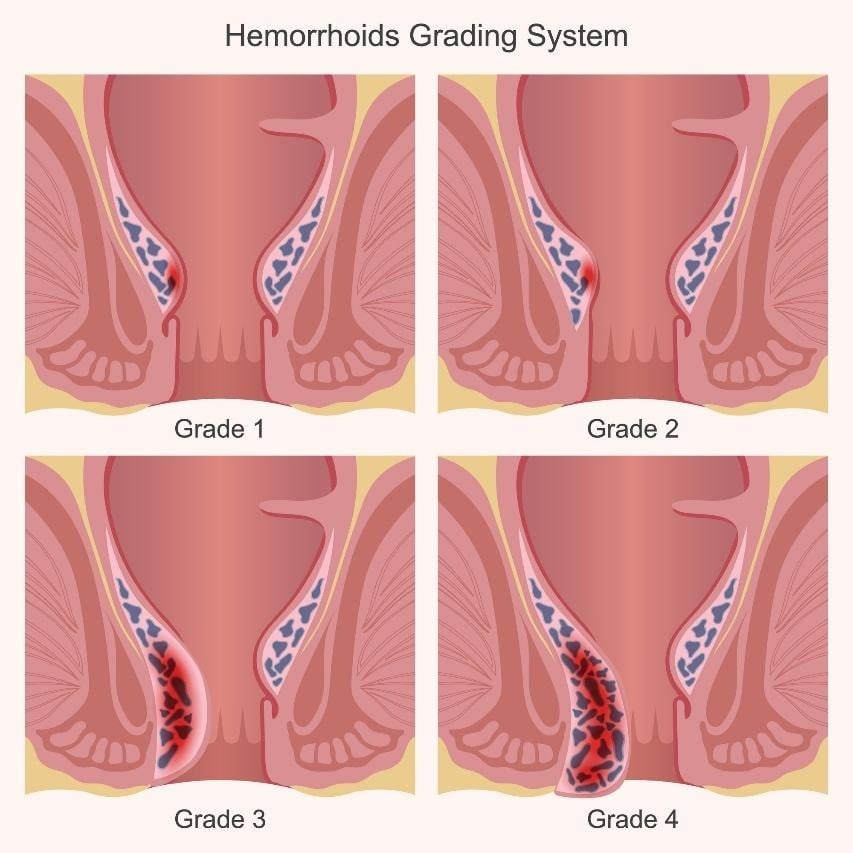
Internal haemorrhoids can be graded based on their degree of severity and how much they prolapse:
-
Grade I internal haemorrhoids - Bleeding occurs, but the haemorrhoid stays inside the anal canal without prolapsing.
-
Grade II internal haemorrhoids - The haemorrhoid prolapses (comes out) during bowel movements or straining but spontaneously goes back in.
-
Grade III internal haemorrhoids - The haemorrhoid prolapses with straining and needs to be pushed back in manually.
-
Grade IV internal haemorrhoids - The haemorrhoid is permanently prolapsed and can’t be pushed back in, often causing constant pain and inflammation.
Higher grades of internal haemorrhoids have a greater risk of complications, like infection or thrombosis (a blood clot forming in the haemorrhoid), and will require different treatments.
Grade I & II internal haemorrhoids may respond to lifestyle and dietary changes, while grade III & IV internal haemorrhoids often need to be treated with a medical procedure, like a haemorrhoidectomy.
Symptoms of haemorrhoids
The symptoms of haemorrhoids can vary, but often include:
-
Bleeding - You may see bright red blood on toilet paper, in the toilet, or in your stool.
-
Itching/irritation - An itchy or irritated sensation in the anal area (called pruritus ani).
-
Discomfort and pain - Aching or pain, especially while sitting or during bowel movements, which can be severe if a clot forms in an affected vein (thrombosed).
-
Tender lumps - Blood clots in veins can cause firm, tender, painful lumps to form around your anus.
-
Mucus - Increased mucus discharge during bowel movements and/or throughout the day, which you see on toilet paper or in your underwear.
-
A feeling of fullness - A lingering feeling that you still need to have a bowel movement.
Generally, internal haemorrhoids cause fewer symptoms – often just some bleeding when passing a bowel movement – but symptoms can be more severe if they begin to prolapse (bulge out of your anus). External haemorrhoids are more likely to cause itching and pain.
If you're experiencing any of these symptoms, it's important to see a healthcare professional for proper diagnosis and treatment.
What causes haemorrhoids?
The direct cause of haemorrhoids is an increase in pressure in the veins in the rectal and pelvic area that results in the veins expanding over time and becoming swollen and enlarged. An increase in vein pressure can happen for a range of reasons, but the most common culprits are:
-
Chronic constipation and frequent straining during bowel movements
-
Prolonged sitting, particularly on the toilet
-
Frequent heavy lifting
-
Pregnancy and childbirth
-
Chronic diarrhoea
-
Ageing, as the tissues supporting the veins naturally weaken over time
What are haemorrhoid risk factors?
The following risk factors can make it more likely that you’ll develop haemorrhoids:
-
Eating a low-fibre diet (which can lead to constipation)
-
Leading a sedentary lifestyle, especially sitting for long periods
-
Being overweight or obese
-
Pregnancy
-
A family history of haemorrhoids
-
A chronic cough
-
Having certain medical conditions, including ones that affect your bowel movements or that raise abdominal pressure, such as liver disease
Understanding what causes haemorrhoids and these risk factors is particularly important after haemorrhoidectomy treatment, as making lifestyle changes can help prevent them from returning.
What is a haemorrhoidectomy?
A haemorrhoidectomy is a surgical procedure performed to remove severe internal or external haemorrhoids. There are different types of haemorrhoidectomies, but they typically involve cutting out the swollen veins, usually under general anaesthesia.
When is a haemorrhoidectomy necessary?
A haemorrhoidectomy is generally reserved for severe cases of haemorrhoids, where more conservative treatments (like lifestyle changes) have already been tried, but have failed to provide adequate relief.
Doctors and surgeons will decide on whether a haemorrhoidectomy is necessary on a case-by-case basis, but you’re more likely to need one if you have:
-
Grade III or IV internal haemorrhoids or large external haemorrhoids causing significant symptoms
-
Mixed internal and external haemorrhoids
-
A failed response to other non-surgical haemorrhoid treatments
-
Persistent bleeding causing anaemia
-
Thrombosed external haemorrhoids (haemorrhoids where blood clots have formed in them)
-
Strangulated haemorrhoids (where the blood supply in the vein is cut off)
-
Symptoms that are severely affecting your quality of life
Conservative haemorrhoid treatments
Before a haemorrhoidectomy is considered, your consultant will typically recommend more conservative haemorrhoid treatments first, such as:
-
Dietary changes, such as increasing the amount of fibre you eat and drinking more fluids
-
Lifestyle modifications, like increasing the amount of exercise you do and reducing how long you sit for
-
Topical treatments, including haemorrhoid creams, ointments, or suppositories
-
Stool softeners
-
Non-surgical haemorrhoid procedures, such as banding, sclerotherapy, or coagulation
Haemorrhoidectomy surgery will usually be considered if a combination of the above has been tried but hasn’t proven effective.
Who is a good candidate for a haemorrhoidectomy?
You’ll likely be considered a potential candidate for haemorrhoidectomy surgery if you have:
-
Severe haemorrhoid/haemorrhoid symptoms that are unresponsive to more conservative treatments
-
Good general health and are considered suitable for surgery
-
Realistic expectations about recovery (your Ramsay team will advise you on what to expect from haemorrhoidectomy recovery)
-
Commitment to post-operative care and making lifestyle changes
Types of haemorrhoidectomy procedures
There are different surgical techniques used for haemorrhoid removal. Your colorectal surgeon will discuss the best approach for your individual case based on your haemorrhoids and situation.
The most common types of haemorrhoidectomy include:
Conventional (excisional) haemorrhoidectomy
Conventional (excisional) haemorrhoidectomies are the most common form of haemorrhoid removal surgery and are typically considered the gold standard, often with the lowest rates of recurrence.
Conventional haemorrhoidectomies involve surgically removing the swollen veins by cutting them away. The surgical wounds may be left open to heal naturally (an open haemorrhoidectomy) or sutured closed (a closed haemorrhoidectomy) based on the location and extent of the haemorrhoids. The surgery is usually performed under general or spinal anaesthesia.
This approach is usually recommended for severe internal and external haemorrhoids. Although it usually yields positive results, recovery can take longer than other forms of haemorrhoidectomy, and post-operative pain may be greater initially.
Stapled haemorrhoidopexy (PPH)
This is a less invasive approach than a conventional haemorrhoidectomy. This approach uses a circular stapling device to reposition prolapsed haemorrhoids. The staples lift and secure the haemorrhoidal tissue back into its normal position and cut off its blood supply.
Less tissue is removed than with the conventional method, generally resulting in less post-operative pain and a faster recovery, although the procedure won’t be suitable for all cases. Haemorrhoids may be more likely to recur than with conventional haemorrhoidectomies.
A stapled haemorrhoidopexy is likely to be recommended for patients with internal haemorrhoids without a significant external component.
Which haemorrhoid procedure is right for me?
Your Ramsay surgeon will recommend the right haemorrhoid treatment for you based on your individual case. They will consider several factors, including:
-
The type of haemorrhoids you have
-
How serious they are
-
Previous treatments you’ve tried
-
Your health and other personal considerations
While a conventional haemorrhoidectomy is usually the most definitive treatment, your surgeon may decide that a stapled haemorrhoidopexy is a better option for you.
The haemorrhoidectomy procedure
Although individual procedures in different Ramsay hospitals can differ in detail, in general, you can expect the following procedure from a haemorrhoidectomy:
Before your haemorrhoidectomy
Assessment - Initially, you’ll have a pre-operative assessment with us, including a review of your medical history, a physical examination, and blood tests if needed.
Bowel prep – You’ll receive guidance on what you need to do before your procedure, but typically you’ll be asked to either use an enema or take laxatives to make sure your bowel is empty. You’ll also receive instructions on fasting beforehand.
Medication - If you take medication, your Ramsay surgeon will advise which to keep taking and which you’ll need to stop taking (such as blood-thinning medication).
Support - We recommend that you arrange for someone to drive you home after your operation, and to stay with you for at least one day as the effects of the anaesthesia wear off.
Stocking up - It’s a good idea to stock up on necessary items before your procedure, including pain medication, stool softeners, high-fibre foods, witch hazel pads, and a sitz bath.
Time off work - You should plan to take time off from work, usually between two to four weeks, depending on the nature of your job.
During the haemorrhoidectomy
Anaesthesia - Depending on the specifics of your operation, you’ll be given a general anaesthetic (you’ll be asleep) or a spinal anaesthetic (anaesthetised from the waist down).
Positioning - You will be positioned to allow the surgeon optimal access to the surgical site.
Duration - The procedure usually takes between 30 to 60 minutes.
Conventional haemorrhoidectomy steps –
-
Once you’re sedated and ready, your surgeon will tie off (ligate) your haemorrhoids to reduce the blood supply to them.
-
Next, they’ll cut away the haemorrhoids (excision).
-
Your surgical wound will then either be left open or sutured closed.
-
A dressing will be applied. In some cases, a gauze pack may be inserted into your anus.
Immediately after your haemorrhoidectomy
Monitoring - You’ll be taken to a recovery room where you’ll be monitored for one to two hours after your operation.
Discharge - Most haemorrhoidectomies are performed as outpatient procedures, meaning you’ll usually go home the same day as your operation, without any need for an overnight stay, unless recommended.
Pain relief - Pain medication will be administered and prescribed for home use.
Instructions - Your Ramsay team will give you instructions about how to manage and dress your surgical wounds, how to use your pain medication, and how to take care of yourself after your procedure.
Follow-up - A follow-up appointment will be scheduled to monitor your recovery and healing.
Haemorrhoidectomy recovery
It’s important to have realistic expectations about haemorrhoidectomy recovery, including how uncomfortable and painful it can be initially.
Haemorrhoidectomies can have a painful recovery, but the pain is usually manageable with the proper medication and care and tends to be the most challenging in the first seven to 10 days.
The first 24-48 hours of your haemorrhoidectomy recovery
You should expect to initially experience moderate to severe pain. During this time, you should:
-
Take your pain medication on the schedule advised (don’t wait for pain to worsen)
-
Start taking stool softeners
-
Rest and limit your activity
-
Stick to a light, soft diet
-
Drink plenty of fluids
Contact the hospital if you can’t urinate within 12 hours (urinary retention).
If you’ve had a gauze pack inserted after your surgery, it’ll usually be removed within 24 hours.
The first week of your haemorrhoidectomy recovery
During the first week, you can expect some pain (gradually decreasing), some bleeding, swelling, and discharge. You should:
-
Continue taking pain medication as prescribed
-
Use wrapped ice packs (15-20 mins at a time)
-
Take warm sitz baths
-
Eat high-fibre foods and drink plenty of water
-
Take small, gentle, frequent walks
-
Avoid prolonged sitting, heavy lifting, or straining
Your first bowel movement: You’ll typically have your first bowel movement within two to four days. If you've been eating plenty of fibre, drinking lots of water, and taking stool softeners, your stool shouldn't be too firm. Try not to strain and allow it to pass naturally without forcing.
Weeks 2-4 of your haemorrhoidectomy recovery
Your pain will gradually lessen, although it will likely still be present. During this time:
-
Continue eating a high-fibre diet and drinking lots of water
-
Keep taking stool softeners - bowel movements will gradually become easier
-
Continue regular sitz baths for relief
-
Gradually increase your activity level
-
Avoid heavy lifting
-
You may be able to return to light work if your job is more sedentary
If your surgical wounds were stitched, the stitches will dissolve naturally. You’ll typically have a follow-up appointment with us during this period to check up on your progress.
Weeks 5-8 of your haemorrhoidectomy recovery
The majority of patients feel significantly better during this period. You may be able to:
-
Return to most normal daily activities and work
-
Resume gentle forms of exercise
-
Stop taking stool softeners, although you’ll continue with a high-fibre diet
You may continue to feel some discomfort during bowel movements, but this should continue to improve.
Your long-term haemorrhoidectomy recovery
Complete healing typically takes 6-12 weeks, with most patients fully recovered by three months, depending on your individual case.
You may still experience some minor symptoms, like itching and mild discomfort for some time, and there may be some scarring. But most patients achieve long-term relief and experience life-changing results.
Pain management strategies after a haemorrhoidectomy
It’s important to understand that haemorrhoidectomies are known to be painful post-operatively, as the area that’s operated on is sensitive and bowel movements will regularly pass through healing tissue. However, pain is manageable with the right strategies.
The pain often tends to be worse around days three to seven, but it will gradually lessen over time as you heal. Pain during bowel movements is expected but improves week by week.
There are several strategies you can use to help manage your pain, including:
-
Pain medication - We’ll prescribe you strong pain medication to take regularly during the first few weeks of your haemorrhoidectomy recovery. Over time, as your pain improves, you’ll be able to transition off prescription pain medication to over-the-counter pain killers like paracetamol and ibuprofen.
-
Sitz baths - A sitz bath is a shallow, warm-water soak that can ease pain and help with healing after a haemorrhoidectomy. Taking regular sitz baths, three to four times a day, including after bowel movements, can help reduce your pain levels.
-
Ice packs - You can try applying wrapped ice to the healing area for 15–20 minutes at a time to help reduce swelling and discomfort.
-
Topical treatments - You can use topical anaesthetics, including creams and sprays, that you apply directly to the healing area to provide pain relief. GTN (Glyceryl Trinitrate) ointment may also be prescribed to relax your sphincter before bowel movements.
-
Following post-operative guidance - Following advice on exercise and activity levels, maintaining a high-fibre diet, and drinking lots of water can all help support your healing and pain management.
Your pain should steadily improve over time – contact your surgeon if your pain is worsening rather than improving.
What are the risks and complications of a haemorrhoidectomy?
Haemorrhoidectomies are generally safe, commonly performed procedures, but as with any form of surgery, there is a risk of complications.
After a haemorrhoidectomy, it’s common to experience:
-
Pain
-
Small amounts of bleeding
-
Swelling
-
Difficulty urinating initially
-
Discomfort during bowel movements
The above are expected and normal after a haemorrhoidectomy. However, if you experience any of the following, you should seek medical attention:
-
Inability to pass urine within 12 hours of the procedure
-
Heavy bleeding (soaking multiple pads)
-
Severe pain not controlled by your prescribed medication
-
Signs of infection (increasing redness, pus, or a bad smell)
-
A fever of 38 °C or above
-
Inability to pass stool
If you have any concerns about your recovery, don't hesitate to contact your surgical team.
Why choose a private haemorrhoidectomy procedure?
Choosing private healthcare for your haemorrhoidectomy means you can access treatment when you need it, as well as these benefits:
- Enhanced privacy and dignity – Your own private room throughout your stay, giving you the comfort and discretion you need during recovery from this sensitive condition.
- Faster access to treatment –Private care means you can schedule your surgery quickly, at a time that suits you rather than being placed on a lengthy waiting list.
- Continuity of care – You'll be looked after by the same consultant from initial consultation through to discharge, building a relationship with a specialist who understands your individual treatment plan.
- Flexible appointments – Appointments arranged at times that work around your busy lifestyle from your initial appointment through to post-operative care.
Haemorrhoidectomy cost
The cost of a haemorrhoidectomy varies depending on the details of your surgery and where you choose to have your procedure.
With Ramsay Health Care, you receive a personalised price for your haemorrhoidectomy after a consultation with one of our surgeons, which will be valid for 60 days.
We offer a range of ways to pay for your haemorrhoidectomy surgery, including:
-
0% Payment Plans – Allowing you to spread the cost of your treatment across our flexible payment plans with fixed, monthly payments over a time period that suits you.
-
Self-fund treatment – All-inclusive Total Care – a one-off payment at a pre-agreed price that covers all the treatment you need.
-
Use your insurance – Your private healthcare insurance may cover your haemorrhoidectomy. You should obtain written confirmation from your insurance provider before starting your treatment with us.
Haemorrhoidectomy at Ramsay Health Care
At Ramsay Health Care, we specialise in colorectal procedures like haemorrhoidectomy, combining expert surgical care with the personalised attention you deserve.
Your Ramsay experience:
-
Convenient locations across the UK, with most hospitals offering free on-site parking.
-
State-of-the-art facilities equipped with the latest surgical technology.
-
Personalised treatment plans tailored to your specific type and severity of haemorrhoids.
-
Patient-focused care from consultation through to discharge
Ready to take the next step? Contact us today to speak to one of our advisors about haemorrhoidectomy surgery at Ramsay Health Care and to book your consultation, you can also research specialists and book online for your consultation if that suits you.


